| Asthma can't be cured but it can be controlled so it does not affect your life. You know that your asthma is under control when:
|
All About Asthma

Did you know that 1 in 7 Kiwi kids have asthma?That’s over 120,000 kids who find it difficult to blow up a balloon or blow out their birthday candles. There’s probably two or three kids who have asthma in classroom, or you may even have asthma yourself! Asthma is not something we talk about often, and we usually don’t even know when someone has asthma; unless it is not well controlled. Sometimes we can see symptoms of asthma when kids are wheezing, breathing heavily, having days off school, or not playing sports. Asthma symptoms usually don't last long, but for some kids, these symptoms can be a daily problem. |
How do I know if I my asthma is under control?
What is asthma?
|
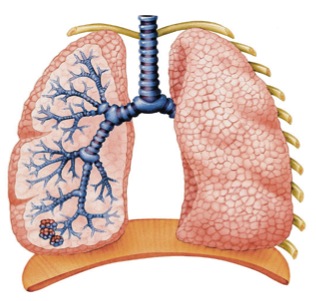
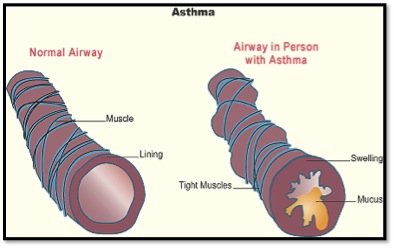
It all happens in the small airways of your lungs called bronchial tubes. When you breathe in, the air goes down these tubes into your lungs. These tubes spread out through all the parts of your lungs, getting smaller and smaller as they go.
When your asthma is under control these airway tubes are clear, and air can flow easily in and out. When your asthma is not under control, the lining of these little tubes is thick, and has lots of sticky mucous (like boogers) sticking to it. This makes the muscles around the outside of the tubes tighten.
When these tubes are clogged up, your chest begins to feel tight, you will have a dry cough, and you will wheeze as you breathe out. You may also find it hard to talk. |
 |
 |
What causes asthma?
- Anyone can get asthma, and it can start at any time of your life
- Asthma can run in the family
- Asthma is much more common in people with allergies
- Pollution and triggers can worsen asthma symtpoms
How is asthma diagnosed?
- Allergy tests: Doctors may test for allergies if they think your symptoms may be caused by this.
- Chest X-ray: This is a picture of your lungs so the doctor can see what is happening inside.
- Peak expiratory flow (PEF): This shows how fast you can breathe out into a peak flow meter when you try your hardest.
- Spirometry: Doctors use this test to diagnose and keep track of asthma. It measures how much air you can breathe into your lungs and how quickly your lungs empty out.
- Exercise or inhalation challenge: This test measures how quickly you breathe after exercise or after taking a medicine.
What are asthma symptoms?
Asthma can make you feel:
- Wheezy (your breath might 'whistle' in and out)
- Short of breath
- Tight in the chest
- Make you cough
What are asthma triggers?
Triggers don't cause asthma (no one knows exactly what does), but they can make your asthma worse or cause an asthma emergency. Knowing as much as you can about your triggers is important, so that you can do try and help reduce these in your everyday life. This may also mean taking a reliever medication prior to coming into contact with known triggers (e.g before exercising).
|
Triggers are different for everyone. Some common triggers are:
|
Other triggers can also include exercise, food additives (including colours and preservatives), fumes, strong smells, chemicals, perfumes, air pollution and smog, some medications, moulds and fungi, and a change of weather or temperature.
Some people also find when their feelings change (they are worried, uptight, stressed, excited or happy), this can make their asthma worse. It’s best to talk to your doctor or asthma nurse if this happens to you a lot.
Remember to watch out for your triggers when your asthma is worse because you will react to them more during this time.
If you want some help figuring out what your triggers are, ask an adult, your doctor or the asthma nurse. Find out more about your triggers here.
How can I manage my asthma?
Along with your medication that your doctor prescribes, it is important to have an Asthma Action Plan to help manage your asthma. This can either be a physical printed copy that you fill in with your doctor, or a digital one using the My Asthma App.
There are two parts to your Asthma Action Plan:
- The first part tells you how to control your asthma long term, which medicine to take, and helps you track your symptoms so you know how well the medicine is working.
- The second part tells you what to do in an asthma emergency, and helps you identify triggers that can cause your asthma worsen.
Asthma emergencies can be life-threatening, but you may be able to prevent them if you follow your asthma action plan. Discuss this with your doctor next time you visit.
Download your free Asthma Action plan here.

How is asthma treated?
Your medicine plays a very important role in keeping your asthma under control. Most kids with asthma have two main types of medication - a Preventer and a Reliever. Some people get confused with the role that each of these medicines has in helping keep our asthma under control. An easy way to remember it is preventers prevent and relievers relieve. To get the most out of your medication, you also need to use a spacer.
Because your medicine is so important in keeping your asthma under control, you need to make sure that you :
- Understand what your different medicines do and when to take them
- Always know where your medication is kept
- Follow the directions for taking the medication
- Always use a spacer when taking your medication
- Make sure that you never run out of medication
Preventer Medication
| Preventer medication does just that - it prevents your asthma.
Preventer medication is probably your most important asthma medication, because it keeps your airways open by stopping your bronchial tubes from getting swollen and inflamed - which stops your asthma getting worse. Preventer medicines work slowly and can take three months of regular use (generally twice a day) before you feel the full benefit of the medicine. It can be dangerous to skip a few doses or stop your preventer when you feel well, as your asthma will often get worse. Preventer inhalers are usually brown, orange, red, or purple. They are generally taken morning and night with a spacer.
|
Combination Medication
|
Combination inhalers contain both a preventer and a long-acting reliever medicine in one device. Some combination inhalers, like Seretide, should not be used in an emergency situation, and you will also require an additional reliever inhaler. However, there is one combination inhaler called Symbicort, which is a 2-in-1 treatment, and is used for both the prevention and relief of symptoms. This must be carried at all times, and you do not need an extra inhaler as a reliever. When your asthma symptoms are worsening, your doctor or asthma nurse will instruct you on how to take it when needed to relieve symptoms and when to seek medical advice in an emergency.
|
Reliever Medication
|
Reliever medication helps you to feel better straight away when you are experiencing asthma symptoms. It brings short term relief as it helps the muscles around your airways relax, so that you can breathe more freely. Relievers are only taken when you need them. Many people rely on their reliever inhaler to feel better immediately, but they do not treat the underlying cause of their asthma -swollen and inflamed airways.
|
Prednisone
Prednisone is a medicine that is taken when you have serious asthma. But it doesn’t work fast - and instead works slowly on the inflamed airways over several hours so that your airways become more open. Prednisone is used for some children for bringing asthma symptoms under control, when your inhalers are not settling your symptoms alone. They bring down the swelling in the lining of the airways and reduce the amount of mucus that is produced.
What is a spacer?
Using a spacer gets 50% more medication into your lungs, so it is very important to use a spacer when taking your inhaler medication.
A spacer is a clear plastic tube with a mouthpiece or mask at one end and a hole for your inhaler at the other end.
A valve in the spacer mouthpiece opens as you breathe in and closes as you breathe out. This helps the full dose of the medicine get into your lungs from the inhaler.
Spacers are free from your doctor or asthma society. Ask your doctor or asthma nurse to show both you and your caregiver how to use a spacer correctly. For more information on spacers click here.

How do I manage an asthma emergency?
It is important that you recognise and treat your worsening asthma as soon as possible – to do this you need to understand what your specific symptoms are. Keep your Asthma Action Plan handy or make sure you and an adult (and this can be your carer, your teacher, your grandparents) understand what actions you need to take when your asthma gets worse.
Mild Symptoms
You might have a slight wheeze, occasional cough, symptoms when excited or running.
You will need need to use your blue reliever or Symbicort combination inhaler, as directed by your doctor or nurse.
Moderate Symptoms
Your symptoms might include finding it hard to breathe and to talk, and a daytime cough, or wheeze, which can upset sleeping at night and no energy. You may need to use your reliever (blue inhaler) with a spacer for immediate relief. You can use up to 6 puffs/doses of your reliever at this time through a spacer (one puff at a time in spacer and take 6 breaths).
Steps for an Asthma Emergency
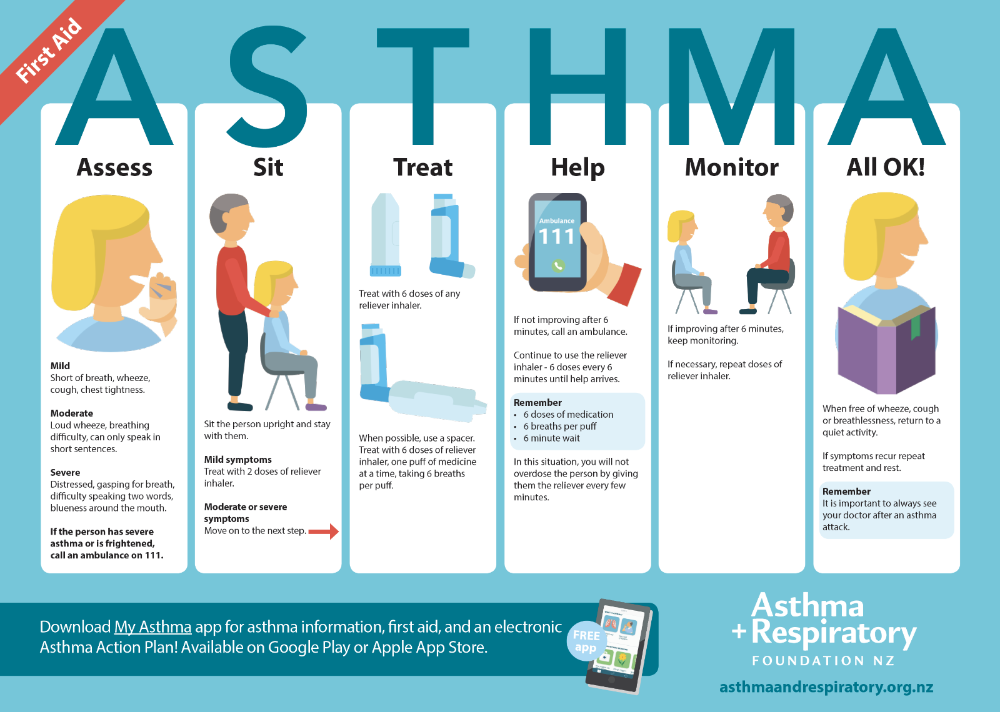
A good way to remember the steps in managing an asthma emergency is to remember the acronym ASTHMA.ASSESS
Mild Symptoms: Shortness of breath, wheeze, cough, chest tightness.
Moderate Symptoms: Loud wheeze, breathing difficulty, can only speak in short sentences.
Severe Symptoms: Distressed, gasping for breath, difficulty speaking two words, blueness around the mouth.
SIT
Sit or lie the person down.
TREAT
Treat with 6 doses of the blue 'reliever' inhaler, preferably through a spacer. One puff of medicine at a time using 6 breaths per puff.
HELP
If not improving after 5 minutes, call the ambulance. Continue to use blue inhaler 6 doses every 6 minutes until help arrives. Remember 6 puffs of medicine, 6 breaths per puff, 6 minute wait
In this situation you will not overdose the person by giving them the reliever every 6 minutes.
MONITOR
If improving after 6 minutes, keep monitoring. If necessary repeat doses of blue inhaler.
ALL OK!
When free of wheeze, cough and breathlessness, return to activity. If symptoms recur repeat treatment and rest. See your doctor.
To download the free Asthma First Aid poster click here.
Important: f you use the combination inhaler called Symbicort, then follow the instructions on your prescription label as well as your doctor or asthma nurse’s written advice on your Asthma Action Plan for what to do when your asthma symptoms are worsening or in an emergency.

-916.png)


